Patient Blood Management is a patient-centered, systematic, evidence-based approach to improve patient outcomes by managing and preserving a patient’s own blood while promoting patient safety and empowerment
Watch the video below – What is Patient Blood Management?
What is Patient Blood Management? Duration: 1:26 点击播放
The Three Pillars of Patient Blood Management
The literature identifies three independent risk factors for adverse patient outcomes: anaemia, bleeding and blood transfusion.
These risk factors are modifiable with the application of the ‘three pillars’ of Patient Blood Management:
- Optimise erythropoiesis (including red cell mass and iron stores)
- Minimise blood loss (surgical) and bleeding (coagulopathic)
- Harness and optimize the patient-specific physiological reserve of anaemia while treatment is initiated
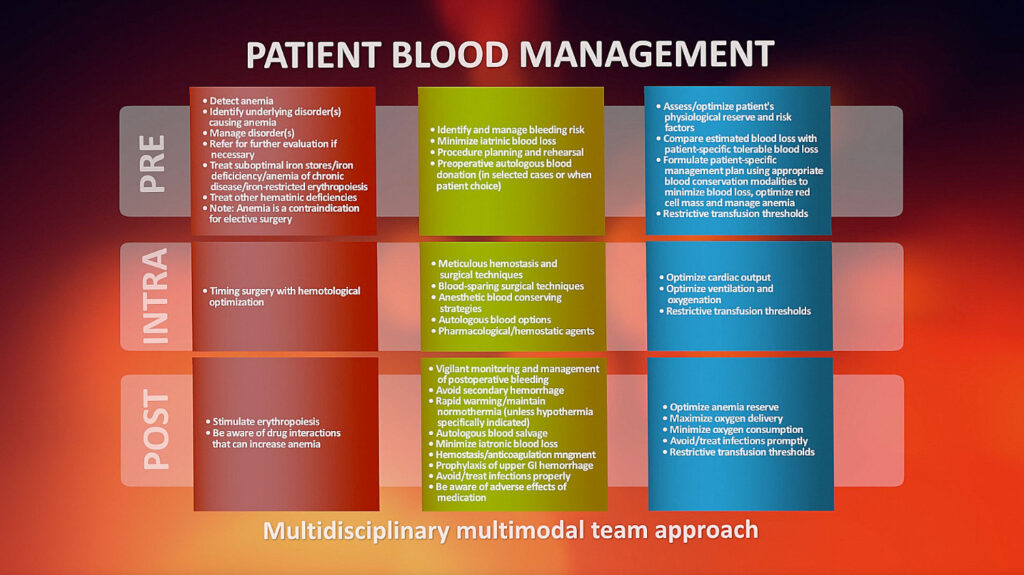
In surgical and medical patients, the three pillars are applied in three phases:
- Before specific treatment (Pre-operative)
- During specific treatment (Intra-operative)
- Following up after specific treatment (Post-operative)
This approach can be represented as a nine-field matrix
Managing the patient’s blood and haemopoietic system is like managing any of the other organs and organ systems during the patient’s care.
Specialists manage the heart, the kidneys, the endocrine system, etc. The patient’s blood requires similar clinical management.
The haemopoietic system and its circulatory products are pivotal for the healthy function of the human organism.
The International Foundation for Patient Blood Management is committed to ensuring that this unique and vital human resource is appropriately managed and maintained in health and disease. To this end, the Foundation promotes scientifically based medical and surgical Patient Blood Management techniques aimed at conserving a patient’s own blood and minimizing or avoiding the need for the transfusion of allogeneic blood components.
The Foundation acknowledges that altruistically donated allogeneic blood, given in trust, is a valuable community resource. However, it is a costly resource with significant potential for adverse clinical outcomes. Accordingly, it should only be used as therapy with patient consent when there is evidence for potential benefit, there are no alternatives, and the risks are appropriately considered and balanced against the benefits.
In this context, the Foundation, as a multidisciplinary organization, is committed to aligning the best medical evidence with ethical and economic considerations that ensure that Patient Blood Management related therapies are appropriately assessed for cost-effectiveness, with patients’ choices and blood donors’ trust being respected.
Prof. James Isbister explains Patient Blood Management (Runs 1:12 Chinese subtitles)